The Future of Sports Injury Rehabilitation
This article was originally published by stack.com and can be found here. Image courtesy of wisegeek.org.
For the past decade, low-level laser therapy has been used more and more in the sports rehabilitation realm to regenerate tissue and stimulate healing. Now, it's being joined by some new kids on the block: plasma and stem cell therapy. According to Stack.com, both are growing more popular as professional athletes publicize their use. Like laser therapy, these two approaches help regenerate injuried areas of the body.
Can you heal a torn hamstring in two weeks instead of six, come back from a ligament sprain in half the time or even return from a severe knee injury without surgery? The answer might be locked in your blood.
In the past five years, a seismic change has occurred in sports medicine as radically new non-operative solutions to difficult problems have emerged. Two of these innovative approaches, platelet-rich plasma (PRP) and stem cell therapy, take advantage of the body’s incredible ability to heal itself. Harvesting these natural blood products and injecting them into injured areas of the body where they are absent can kick-start the regeneration process, leading to faster recovery and fewer re-injuries
Sound familiar? Professional athletes, including Peyton Manning, Tiger Woods, Rafael Nadal and Kobe Bryant, have used PRP to recover from career-threatening conditions.
What is PRP?
PRP is the most popular of the new blood-spinning techniques and perhaps the best understood.
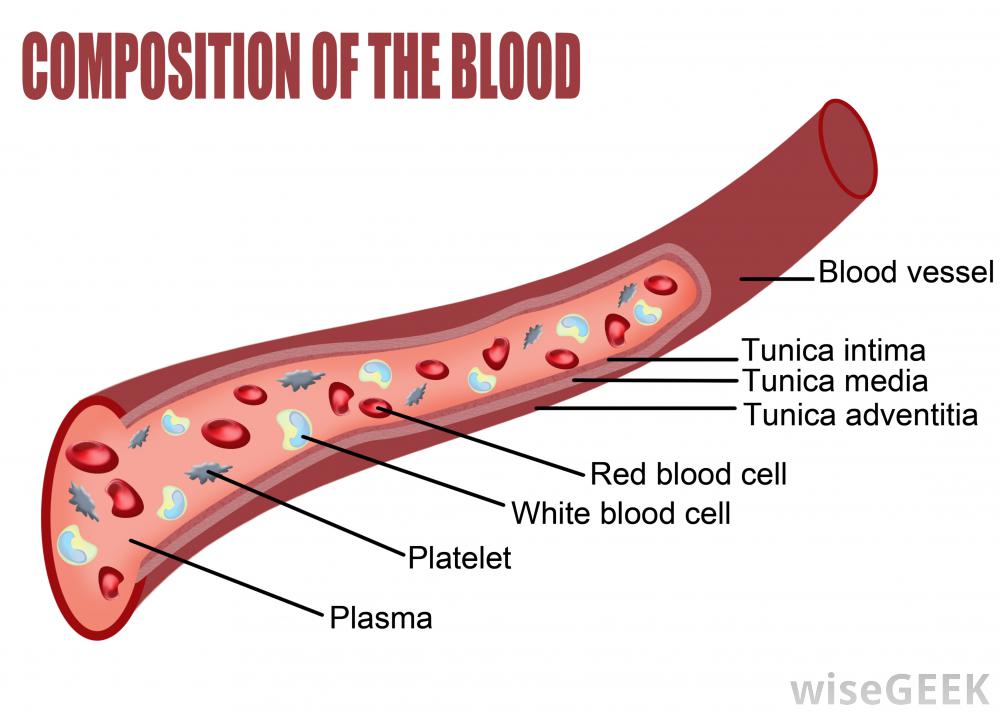
Platelets, like white cells and red cells, are normal blood components. Platelets are critical to healing because they contain the body’s cell- and tissue-building proteins. By drawing a standard blood sample and then concentrating it in a centrifuge, the amount of these powerful growth factors skyrockets.
The problem with many injuries is that blood flow is disrupted, and the normal healing cycle slows down or stops. When the PRP concentrate is injected into injured tissue, the platelets activate and release their growth factors. This immediately cuts down inflammation and ramps up new tissue growth. This reboots the healing cascade, but can take two to three more weeks for complete healing. Precision of the PRP shot is very important, and it usually requires the use of an ultrasound or live X-ray guidance system.
Research has shown that PRP effectively treats tennis elbow, Achilles tendonitis and hip bursitis. New data also demonstrates that PRP can accelerate recovery from ankle sprains, hamstring strains and collateral knee injuries. The most promising, but controversial, use of PRP may be in the treatment of painful knee arthritis.
What is Stem Cell Therapy?
After the early clinical success seen with PRP, researchers began looking to exploit the natural healing benefits of circulating stem cells. These are immature cells in the body that develop into any type of specialized tissue after they are activated by local growth factors. For example, the same stem cell  can grow up to create bone, muscle or ligament, based on where it is injected.Whereas newborns have the highest percentage of stem cells, adults still retain some circulating stem cells in blood, fat and bone marrow. New techniques of harvesting and managing these adult stem cells are now being investigated for use in accelerating recovery from injury.
can grow up to create bone, muscle or ligament, based on where it is injected.Whereas newborns have the highest percentage of stem cells, adults still retain some circulating stem cells in blood, fat and bone marrow. New techniques of harvesting and managing these adult stem cells are now being investigated for use in accelerating recovery from injury.
Current U.S. regulatory laws prevent stem cells from being manipulated with the use of lab-added hormones or growth factors, although this is allowed in other countries. Most stem cell injury therapy in the U.S. has focused on bone marrow aspiration (BMA) to gather the highest possible number of stem cells possible. A bone marrow sample is drawn from the pelvic bone under local anesthesia and the sample is filtered and centrifuged like PRP. The BMA concentrate is then injected into the injured tissue to stimulate healing.
Research has not fully determined the effects of stem cell injection for injured muscle, cartilage or tendon, but the treatment appears to be safe, and the outlook is promising. In some cases, PRP and BMA are being combined to address difficult problems such as rotator cuff tears, ACL injuries and complex broken bones.
The use of PRP and BMA represent the leading edge of an entirely new way of approaching athletic injuries without surgery, along with cold laser therapy. The body is an amazing machine, but sometimes it needs some help, and surgery is not always the best approach. Although cellular treatments like PRP and BMA are not needed for most minor injuries, they are now available to deal with more challenging problems.
The good news is that an increasing number of orthopedic clinics offer PRP and BMA injections. The bad news is, like most new treatments in medicine, your insurance company will probably not pony up to pay for it. That means you will likely have to part with some of your hard-earned cash to grab this piece of the future today.


.webp)