Plantar Fasciitis Treatment using a fluid motion approach
Plantar fasciitis can be a very debilitating issue. Frustration sets in because many home remedies and suggestions from practitioners may not be all that helpful. Here are five tips for practitioners to address the function of why a patient’s pain is in the foot using a fluid motion approach.
1. Rule out a heel stress fracture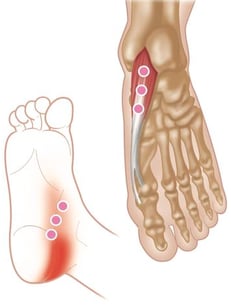
Plantar fasciitis patients are in a decreased functional state, allowing for more severe symptoms to be present. The site of pain in a stress fracture is usually deep and typically does not improve throughout the day. A calcaneal squeeze test1 can be a very important test to direct the practitioner to order x-rays and consider a conservative treatment regiment. If the heel pain doesn’t get dramatically better, then an MRI is warranted.
2. Understand the function of gait in the foot
In many educational documents, patients receive or read the information that plantar fasciitis is caused by the tearing of ligaments from the calcaneus due to walking, running or excessive standing. Let's dig deeper in to the functional anatomy of the foot; a strain of the plantar fascia can present from a break down in the three phases of the gait of the foot: rear, mid, and fore foot. When the calcaneus hits the ground in a locked neutral position, this activates a proper internal tibial rotation and activates the muscles to transfer weight to the 1st ray (medial foot) and transfers weight to the great toe for the push off phase of gait.
At that point the windlass effect of hicks2 stresses the plantar fascia and deep muscles of the foot to compress to the metatarsals cuneiform and navicular (arch of the foot) to form the “arch of stability” to properly transition weight in the propulsion of gait. In repetitive motion injuries, such as marathon training or wearing improper footwear with a pronated or supinated foot, this mechanism is compromised and the plantar fascia becomes stressed at the beginning and end of the gait cycle, leading to stress reactions and micro tearing. Without proper evaluation of the foot during gait we may never address the root cause of the issue and the patient will suffer the consequences.
3. How to treat the foot when it is actively inflamed
Let’s look at a scenario that presents a patient who has been suffering with foot pain for  the past few weeks. The patient may present having trouble bearing weight in the morning but after 10 steps and a light calf stretch they can get into a pair of shoes and the foot pain is bearable throughout the day. When sitting for an extended period of time, however, the pain returns upon standing. As the patient is examined, the tenderness of the foot is much worse than expected and the gait evaluation is compromised by the foot pain.
the past few weeks. The patient may present having trouble bearing weight in the morning but after 10 steps and a light calf stretch they can get into a pair of shoes and the foot pain is bearable throughout the day. When sitting for an extended period of time, however, the pain returns upon standing. As the patient is examined, the tenderness of the foot is much worse than expected and the gait evaluation is compromised by the foot pain.
Where do we start? Many times, the practitioner will support the foot and reduce activity until the symptoms are reduced enough to properly treat the foot. However, in many scenarios, this can lead to a prolonged time and the patient can easily get frustrated. With the FMST instruments we can address the plantar surface of the foot lightly in a dorsiflexed (stretched) and plantar flexed position to evaluate the ability to essentially “push” excess interstitial fluid from the region in a patient comfort position without excessive work on the foot with a light angular scanning technique. Essentially feeling the fascial glide and reducing mild skin/fascial adhesions. If the foot needs to be plantar flexed to the patient’s comfort, we will address a little deeper into the plantar fascia and fascial connections of the deep intrinsic adductor, flexor and abductor muscles of the foot. Be conservative with the time spent in the region of the medial foot.
4. Dynamic plantar treatment
With the patient in a supine position, the practitioner can address the plantar fascia in a pattern of movement based treatment with the FMST instruments. First, apply a scan to the plantar surface of the foot in and passive plantar flexion to dorsi-flexion movement with patient relaxed. By identifying the region of greatest tissue dysfunction in a passive movement, the practitioner can activate the flexors and extensors of the foot, applying the FMST instruments with resisted active ROM throughout the movement. Initially if the plantar fascia is too sensitive the patient can actively extend the ankle while treatment is applied to the plantar fascia in an active inhibited pattern for maximum effectiveness and improved patient comfort. Never spend more than 30 seconds to three minutes of active treatment to the affected area to reduce further injury to the plantar region.
5. Addressing the lower extremity and pelvis for dysfunction attributing to plantar fasciitis
In many cases the gastroc-soleus complex can be a great help to addressing issues in the foot. Altered core and pelvic/hip function can lead to changes in foot biomechanics and over time a breakdown can present as a plantar issue. Most cases of foot 
dysfunction are secondary breakdowns of the kinetic chain as they allow fascial changes and in the posterior chain. In this case, we will address the gastrocnemius in a triplanar soft tissue mobilization with the FMST instruments. Start with the patients’ foot dorsiflexed on a slant board and apply angular pressure inferior to superior as the patient performs a sagittal, coronal and transverse ankle mobilization technique. Each movement should be performed 10-15 reps allowing an increase in ankle mobilization and increase an in fascial glide of the lower calf region. This technique although a little more involved can be applied to the soleus as well.
In many office settings, this technique can be supported with proper fitting insoles and taping techniques as well as passive therapy when warranted. Our goal in a plantar fasciitis case is to see a reduction of the frequency and intensity of the patients’ symptoms as well as an improvement of the primary dysfunction to reduce the duration of the patients’ pain cycle. With any plantar fasciitis case, they can be difficult and time consuming in the office. So with these simple techniques a practitioner can improve their treatment times and reduce the patients duration of a very frustrating condition.




.webp)

